Ten years may sound like a long time, but some days, it feels like yesterday. This May 13 was ten years since I had my brain tumor surgery. I feel proud to have been able to accomplish and experience so much in my recovery. But I also feel blessed to be able to share my growth and achievements with my family and friends. We have all celebrated jobs, promotions, graduations, weddings, holidays, and birthdays and welcomed new members to our families while saying goodbye to loved and cherished ones. We faced hardships, challenges, and painful reminders of the loss of loved ones as well as the loss of oneself as our bodies and abilities may have changed.
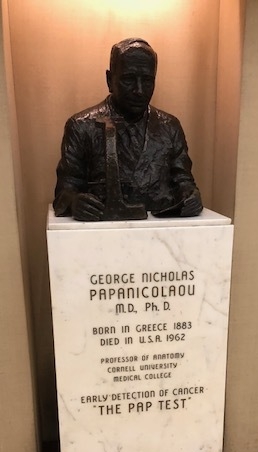
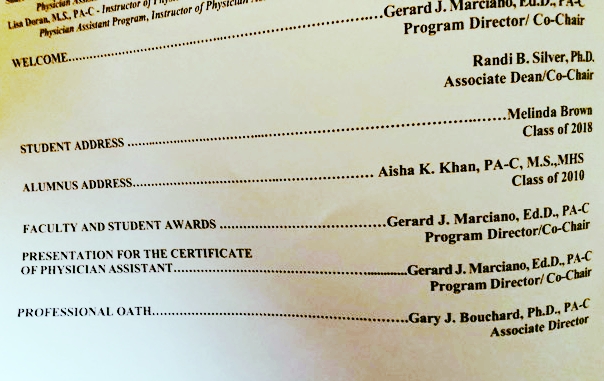
I remember vividly sitting in my room at Gaylord Rehabilitation in Wallingford, CT, at 32 years old, imagining who I would be ten years later at 42. It started with picturing myself six months from then, walking again, being hired at the job I wanted desperately, and standing in front of the classroom. To wear the white coat again, smell alcohol wipes, and print patient lists. With determination and the help of an excellent medical team, beautiful friends, and family, all of that has happened, and so much more. I found kindred spirits and was told I am now a survivor, joining efforts to promote brain tumor awareness locally with the Connecticut Brain Tumor Alliance so others could turn to this community. I wrote articles about recovery and brain tumor awareness published in online media. I traveled to Chicago to volunteer at the American Brain Tumor Association, connect with others affected by this diagnosis, and advocate nationally. I’ve had the privilege of teaching at two Physician Assistant Programs. I ultimately returned to my alma mater and developed a deeper appreciation for Halloween with a few noteworthy costumes, often joined by students and colleagues.
I could not drive for a year, only to board planes and travel internationally to France, England, South Africa, Australia, and domestically to Hawaii to celebrate a wedding with good friends. I moved to a new city, afraid to walk its busy streets, only to be walking onto stage two years later at the Tory Burch Foundation Embrace Ambition event to speak to a live audience of over 1000 attendees about living with a disability and believing in yourself. I completed a doctoral degree, was promoted, and was recently asked to be associate program director for an interprofessional program involving the medical college and physician assistant program.
All this happened in the blink of an eye over the past ten years. To my community of friends, family, colleagues, and survivors, take a moment to reflect on the last ten years of life. Celebrate with our journey and the memories we have made. Let’s acknowledge our celebrations, losses, misses, and hardships that we have overcome and still do.
I haven’t finished yet; I’m already planning for the next ten.